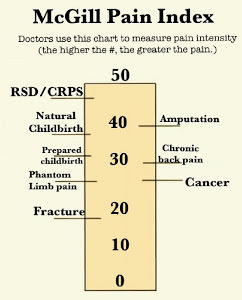
The last five weeks have been an uphill battle, with far too much of it spent in the hospital. My sickness reached a point where I couldn’t keep fluids down, my electrolytes were out of balance, I was fighting another infection, and my body rejected almost every medication. As I’m currently in my third trimester, this was more than just uncomfortable; it was a serious concern.
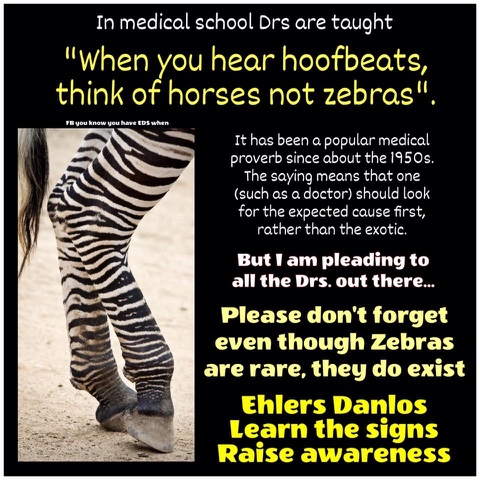
When I was first admitted, we were hopeful. The medical team tried two different anti-sickness IVs and even steroids, but nothing made a difference. My body wasn’t tolerating anything. Eventually, the dieticians came to see me to create a plan to get some much-needed nutrition into me. However with Drs unable to agree with each other on cause – alternating between putting it down to a late appearance on Hyperemesis or a flarr up of my Gastroparesis, it became difficult to create a plan to follow.
This is where things started to go dramatically wrong.
Despite being reassured by the dietician that the Ensure Juice they provided was dairy-free, I went downhill almost immediately. My vomiting worsened, my brain fog intensified, and all my usual allergy symptoms flared up. The medical team dismissed my concerns, insisting these were just part of my condition. After several days of this, I asked to see the bottle myself. There, in clear, bold letters, were the words: Milk Protein.
I immediately stopped drinking it and demanded to speak to the dietician. When she arrived, she insisted my notes said I was lactose intolerant, not that I had a milk allergy—a distinction I had clearly emphasized in our previous conversation.
After an urgent meeting with the multidisciplinary team, the decision was made to place a nasojejunal (NJ) tube. This tube goes through the nose, down the throat, and into the intestine, bypassing the stomach completely. It was supposed to be a solution, but even getting the tube placed took nearly a week because the ward couldn’t provide the necessary care, and the receiving ward kept refusing the referral.
Once the tube was finally in, a nutritional feed was started. About an hour in, my vomiting increased again, and I started to feel a sense of déjà vu. I checked the ingredients. In bold letters, once again, were the words Milk Proteins. It felt completely inconceivable that this same mistake could happen twice.
I called the dieticians again, and this time, they informed me they couldn’t find a suitable feed for my allergies. I pointed out that a quick two-minute Google search brought up several options, but they explained they didn’t have contracts with the suppliers, so they couldn’t prescribe them.
Instead, they suggested trying a different high-calorie nutritional drink. We carefully went over the ingredients, and it seemed safe. Within minutes of trying it, I went into anaphylactic shock. My throat started to close, my heart rate skyrocketed, and I couldn’t breathe. Thankfully, a nurse was in the bay and immediately passed me my Epipen which I administered. The Epipen saved me, but we still have no idea what caused the reaction. It’s now simply labeled as an “unknown new allergy.”
At that point, I was discharged home with no feed. The plan was for me to push fluids and manage my medication through the tube on my own. I was happy to leave—I had lost all confidence in the hospital. We even managed to go on holiday, balancing making memories with my children and trying to manage the extreme fatigue.
A community dietician visited us not long after we got home. We made a plan for a soya-based feed and a pump. I was optimistic. But that optimism lasted only a few hours. I received a phone call informing me they had arranged for me to be readmitted to the hospital due to my continued vomiting, poor blood results, and significant weight loss. I was devastated.
I’m now back in the hospital, waiting for the daily doctor rounds, hoping they will discharge me. But in all honesty, I have little faith left. I’m currently on a soya-based feed we had to buy privately, but at over £160 a week, this isn’t a long-term solution.
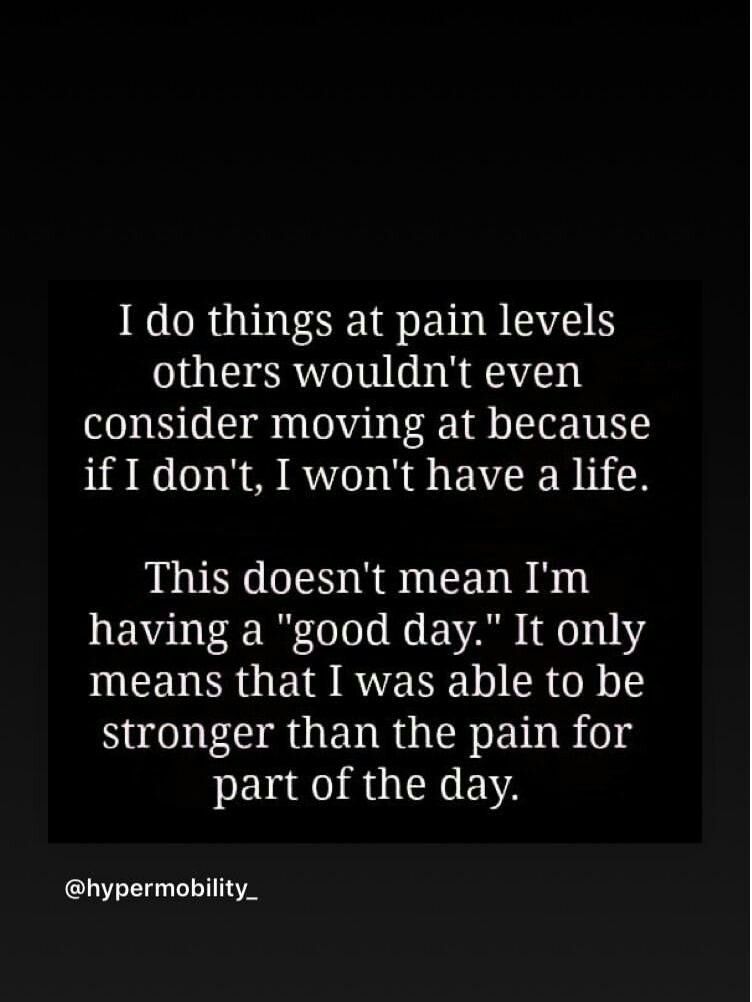
My mental health has been impacted massively. I’m exhausted and I just want to be home with my family. Between these repeated failures and having to constantly advocate for myself—including after a nurse spent ten minutes passionately telling me I could be cured if I simply changed my diet, took supplements, and prayed hard enough—I am at my wits end.



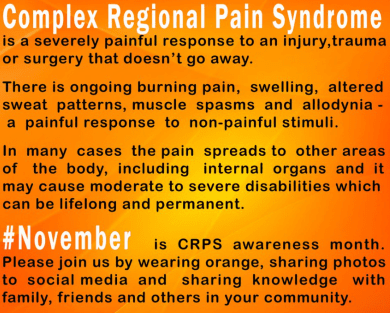

 Today I was up in London to see my neurologist to get my six weekly injections. I was looking forward to speaking with him as this time round my botox had been 7 weeks apart. Normally this would have resulted in severe facial, neck and arm spasms but for a change I have been okay. It is only over the last few days that I have felt the familiar tugging sensation around my eyes, jaw and neck. Whilst I have had spasms in these areas it has been easy to cope with. My arm has been spasming/twitching more but still at what I consider an acceptable rate, so I was eager to discuss with him aiming for 7 weeks again. Now as luck would have it he’s not working that day in 7 weeks time, so my appointment is as usual in 6 weeks, but this something I would like to aim for.
Today I was up in London to see my neurologist to get my six weekly injections. I was looking forward to speaking with him as this time round my botox had been 7 weeks apart. Normally this would have resulted in severe facial, neck and arm spasms but for a change I have been okay. It is only over the last few days that I have felt the familiar tugging sensation around my eyes, jaw and neck. Whilst I have had spasms in these areas it has been easy to cope with. My arm has been spasming/twitching more but still at what I consider an acceptable rate, so I was eager to discuss with him aiming for 7 weeks again. Now as luck would have it he’s not working that day in 7 weeks time, so my appointment is as usual in 6 weeks, but this something I would like to aim for.