Over the last few years I’ve not had the best experiences at my local hospital. I’ve gone in incredibly sick and been discharged in a worst state multiple times. It’s got to the point now where I have to know in myself that I can no longer cope at home before I will agree to go.
The other night after spending several hours vomiting uncontrollably, passing blood, and doubled up in pain so severe I was unable to talk through it or focus my partner rang an ambulance. I dislocate multiple times a day and live with organ prolapse, I’m good at handling pain but this was another level of hell.
The ambulance we would end up cancelling as it was several hours away and family could drop me there quicker. I was sat in my chair, throwing up, crying in pain and quite frankly not coping. A few hours into the wait I seized. I don’t remember this. The doctor the next day told me I’d managed to seize out my wheelchair onto the floor, they’d had to scoop me up and get me round to resus.
I can remember throughout the night they attempted multiple times to place a cannula but failed. I desperately needed meds and fluids, and asked for them to use an ultrasound machine and ideally a consultant as my veins are extremely hard to find but also blow very easily due to my Ehlers-Danlos syndrome. This request was ignored and they decided not to administer the fluids or meds I needed. I was there for over 12 hours. Eventually they decided to take blood from an artery by my groin. Again I requested an ultrasound and experienced Dr such as the anaesthetist on call (they are used to my veins and are patient) instead they pressed ahead blindly and painfully.
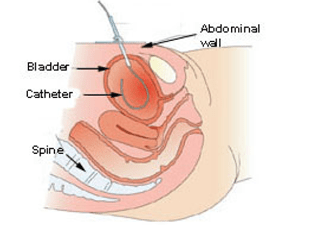
I’ll delve into this topic another time in more detail but please understand that a disabled person’s medical aids are an extension of themselves. You should never touch them without first gaining consent. While I was in the hospital I had the valve removed from my Cathater. They did not have my consent to do this. They had asked to attach a bag which was fine, I attach bags to the valve all the time. But I would never consent to the removal of the valve as then I would be on free flow which would cause horrific spasms as I have a neurogenic bladder. The valve is the only thing that helps manage these spasms. Yet it was taken off and binned without consent.
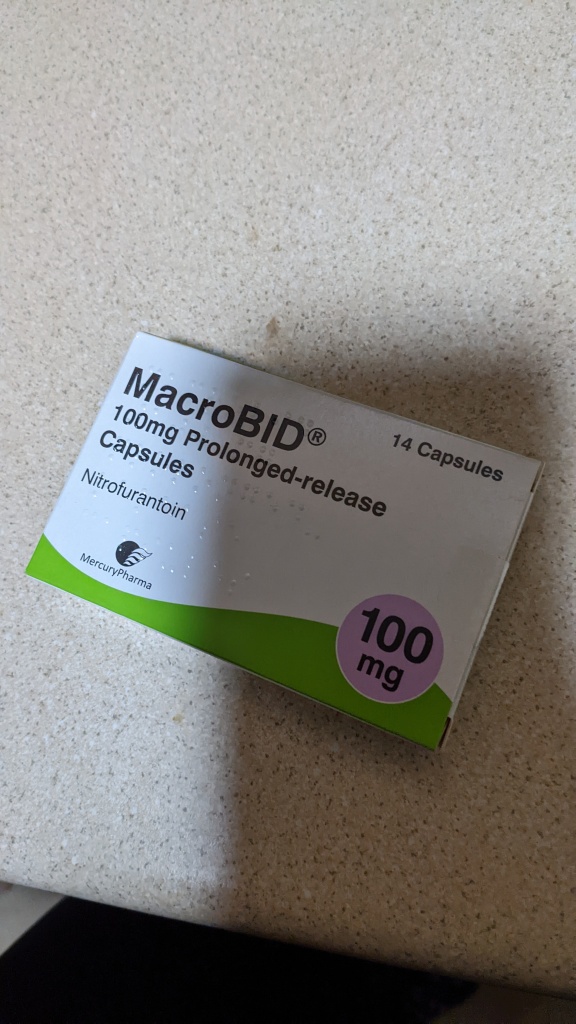
I was discharged that morning and handed a few days worth of the same antibiotics I had just finished and sent home. When my partner arrived in resus to collect me the first thing he asked was if I was well enough to go home. I shook my head but said nothing. Within an hour of being home my district nurses were calling another ambulance for me. My temp was 39.5, I couldn’t stop shaking and I was still in agony. There was a four hour wait and with how concerned my team were Damon loaded me back into the car.
This time they listened a bit better. We established that actually my bloods had shown a kidney infection and I needed a completely different set of antibiotics. But was once again sent home. Today I’ve hardly stayed awake. My other half stayed home to look after me and has had to wake me up for my nurses and meds. I’m exhausted, still with the raging temperature and just frustrated.